Immunocore’s immune-based therapy could be part of a functional cure strategy for HIV and potentially for hepatitis B.
An experimental bispecific T-cell engager, which helps immune cells attack HIV-infected cells, may help reduce the viral reservoir and enable long-term remission, according to results from a small study presented at the Conference on Retroviruses and Opportunistic Infections (CROI 2025).
Immunocore’s MC-M113V was well tolerated and associated with slower viral rebound or HIV control in 20% of study participants, compared with a historical rate of about 5% for untreated people, Beatriz Mothe, MD, PhD, of the Spanish HIV/AIDS research organization IrsiCaixa, reported.
“I look forward to further data from the trial at higher doses, as part of wider efforts to find solutions that could enable people with HIV to remain healthy without lifelong antiretroviral treatment,” Mothe said in an Immunocore news release.
Antiretroviral therapy can keep HIV suppressed indefinitely, but the virus inserts its genetic blueprints into host cells and establishes a long-lasting reservoir that is very difficult to eradicate. Researchers have explored numerous cure approaches—from broadly neutralizing antibodies to CRISPR that cuts integrated HIV DNA out of cells to stem cell transplants from donors with a rare protective mutation—but to date, there are no reliable and accessible therapies to bring about long-term remission.
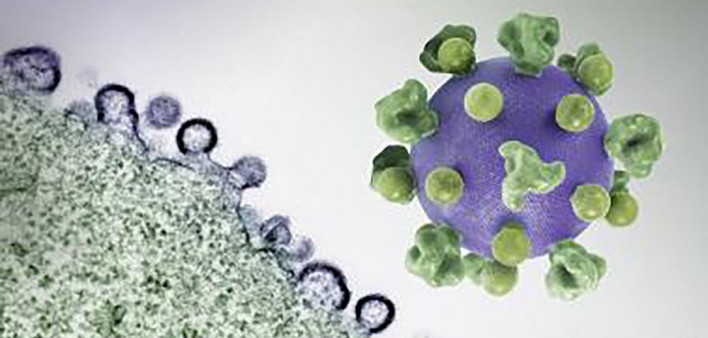
MC-M113V is a bispecific T-engager, an engineered antibody-like molecule that attaches to both CD8 killer T cells and HIV proteins expressed on infected cells, forming a “bridge” that enables the killer cells to eradicate the infected cells. Specifically, MC-M113V binds to the CD3 protein on CD8 cells and HIV’s gag protein displayed in HLA complexes on the surface of CD4 helper T-cells containing integrated virus. This bridging helps overcome T-cell exhaustion, Mothe explained.
A similar approach is already being used to treat cancer. In 2022, the Food and Drug Administration approved Immunocore’s Kimmtrak (tebentafusp) for a rare type of melanoma affecting the eye. This bispecific binds to both the CD3 receptor on killer T cells and specific melanoma antigens. The company calls its cancer platform “immune-mobilizing monoclonal T-cell receptors against cancer,” or ImmTAC, while the antiviral version is dubbed “immune-mobilizing monoclonal T-cell receptors against virus,” or ImmTAV. Immunocore is also testing this approach for hepatitis B.
The Phase I/II STRIVE trial presented at CROI included 16 HIV-positive men with a specific HLA pattern (HLA-A*02:01). The average age was approximately 33 years. They had been living with HIV for about five years and had been on stable antiretroviral therapy with viral suppression for most of that time. However, individuals who started antiretrovirals less than 12 weeks after acquiring HIV were excluded, as this group is more likely to have natural viral control. They had a current CD4 count above 500 and had never fallen below 200.
The participants received escalating doses of IMC-M113V administered via IV infusion once weekly for 12 weeks. Five men received a 60 microgram dose, five received 120 mcg and six received 300 mcg. They then paused their antiretrovirals in an analytical treatment interruption for 12 weeks, resuming if their viral load rose or their CD4 count fell below 350.
During the treatment interruption, laboratory tests showed changes in cytokine levels consistent with T-cell activation. There was a decrease in cell-associated HIV gag RNA and a trend toward a drop in intact HIV DNA, suggesting reduction of the viral reservoir. M113V was no longer detectable in the blood at 12 weeks, suggesting that the immune system was learning to fight HIV on its own.
Most of the 15 evaluable participants experienced viral rebound as expected after stopping antiretrovirals. However, one person taking the 120 mcg dose and two taking the 300 mcg dose showed evidence of viral control. These men experienced initial viral rebound, but their viral load then fell to a low level (around 200 copies or less) at eight weeks. One person remained off antiretrovirals for eight weeks, and two did so for the full 12-week treatment interruption period.
“This observation of initial viremia followed by control at week 12 is typically observed in less than 1% of all people living with HIV,” Immunocore noted in its news release. “Such ‘regained’ post-treatment control may be associated with an immune response to the virus.”
IMC-M113V was generally safe and well tolerated with no serious adverse events. T-cell therapies can cause cytokine release syndrome (CRS), which can lead to inflammation throughout the body. Most people in the highest-dose group experienced mild CRS, characterized by fever lasting a few hours after the first dose. There were no treatment-related discontinuations, though one person dropped out early for unrelated reasons.
“This study provides the first evidence of antiviral efficacy for this novel mechanism of action,” the researchers concluded.
The STRIVE trial is ongoing, evaluating IMC-M113V at doses higher than 300 mcg and longer treatment interruptions. Gilead Sciences is also testing a bispecific T-cell engager, GS-8588, now in a Phase I trial after promising laboratory and animal findings.
Most experts don’t think bispecific T-cell engagers or other immune-based therapies will cure HIV alone, but they may one day be part of a combination strategy for long-term remission, sometimes called a functional cure.
Click here for more news about HIV cure research.
Click here for more news from CROI 2025.
- #antiretrovirals
- #bispecific T-cell engager
- #CROI 2025
- #Cure
- #functional cure
- #HIV
- #HIV treatment
- #IMC-M113V
- #immunotherapy
- #remission
- #reservoir