About 80% of patients with a specific genetic mutation experienced complete remission and avoided surgery, chemotherapy and radiation.
Most people with mismatch repair deficient (dMMR) cancers who used the checkpoint inhibitor Jemperli (dostarlimab) were able to forego surgery and maintain their quality of life, according to study results presented this week at the American Association for Cancer Research annual meeting (AACR 2025) and published in The New England Journal of Medicine.
All 49 patients with rectal cancer who completed a six-month course of immunotherapy experienced a complete response without surgery, chemotherapy or radiation, as did two thirds of those with other dMMR malignancies, senior study investigator Andrea Cercek, MD, of Memorial Sloan Kettering Cancer Center, reported.
“These findings are very important for patients with early-stage dMMR tumors because it’s likely they do not need surgery or radiation if they are treated first with immunotherapy for a sufficient amount of time,” Cercek said in an AACR news release. “Surgical resection can be complicated and risky, especially in organs such as the stomach, pancreas or rectum, so this approach can lead to organ preservation, which offers a better quality of life as well as a potential survival benefit.”
“These results could change how we treat some cancers,” added lead investigator Luis Diaz, Jr, MD, of Memorial Sloan Kettering. “Current treatments like surgery, radiation and chemotherapy can seriously affect quality of life. For example, treating rectal cancer this way can lead to infertility and problems with bowel, bladder and sexual function, as well as other daily challenges.”
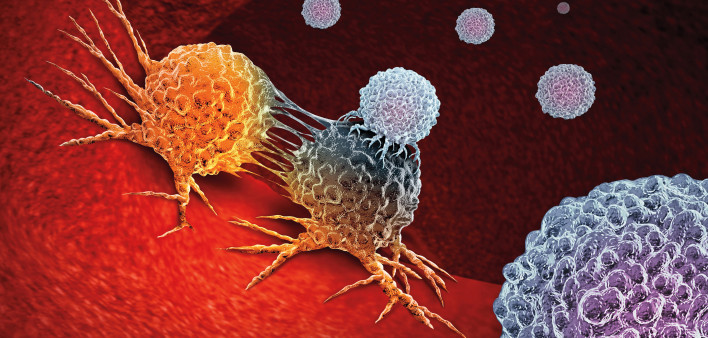
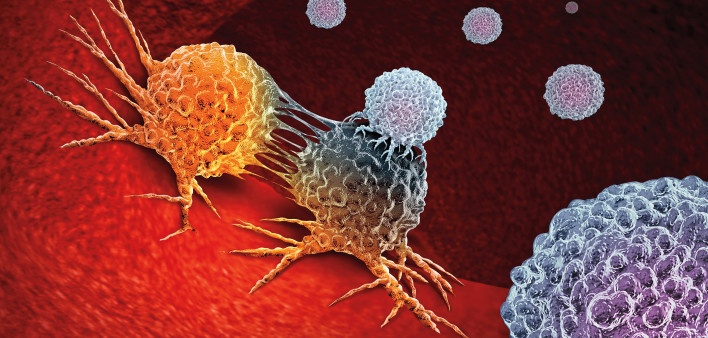
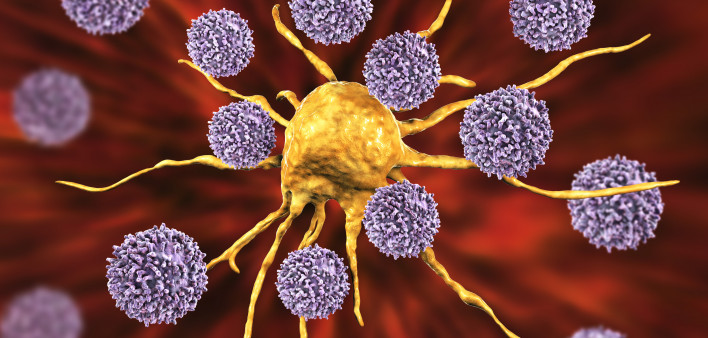
Jemperli, from GSK, is a monoclonal antibody that targets PD-1, a receptor on T cells that regulates immune function. Some tumors can hijack PD-1 to turn off immune responses, and drugs that block the interaction between PD-1 and its receptor on cancer cells can restore T-cell activity.
The Food and Drug Administration first approved Jemperli in 2021 for people with advanced or recurrent endometrial cancer. Later that year, the drug received accelerated approval for advanced or recurrent dMMR solid tumors, regardless of location, that have progressed despite prior treatment.
Normally, cells can detect and repair mistakes that arise when DNA is copied during cell division, but tumors with mismatch repair deficiency lack this mechanism, meaning mutations can accumulate and allow malignant cells to grow out of control. Around 5% to 10% of rectal tumors are mismatch repair deficient. This study highlights the importance of genomic testing to see whether patients are likely to respond to immunotherapy.
Jemperli made headlines at the 2022 American Society of Clinical Oncology annual meeting when Cercek reported that all 12 patients with locally advanced rectal cancer who completed six months of treatment achieved complete remission. Two years later, she presented results from a larger group of 42 patients in the Phase II study, again reporting a 100% response rate. Most participants were cancer-free for at least a year, with some of the original patients still in remission for up to four years.
The trial (NCT04165772) was then expanded to include people with other types of cancer. This analysis included 117 previously untreated patients at Memorial Sloan Kettering. They had Stage I, II or III dMMR solid tumors that were eligible for potentially curative surgery. A majority were women, and most were white.
Cohort 1 consisted of people with rectal cancer, which is similar to colon cancer; the two are often combined—colorectal cancer—in clinical trials. Some had Lynch syndrome, a genetic condition that leads to mismatch repair deficiency and dramatically raises the risk of colorectal cancer. (Rectal cancer is distinct from anal cancer, which is usually caused by human papillomavirus.) The patients in cohort 2 had various malignancies, including bladder, bile duct, colon, endometrial, esophageal, prostate and stomach cancers.
The study participants were treated with Jemperli alone for six months. Those who experienced a complete response could opt for nonoperative management, while those with residual disease were scheduled for surgery.
All 49 rectal cancer patients who received the full six-month course of treatment had a clinical complete response and chose nonoperative management. In the second cohort, 35 of the 54 patients who finished treatment (65%) had a complete response, 33 of whom opted to forego surgery. Case numbers were small for the other cancer types, but those with esophageal, stomach and prostate cancer had less robust responses. In both cohorts combined, 84 of the 103 people who finished treatment (82%) had a clinical complete response, and 82 did not undergo surgery. Among the initial rectal cancer patients with longer follow-up, the recurrence-free survival rate at two years was 92%.
People with lower levels of circulating tumor DNA during treatment were more likely to experience complete remission after six months of treatment. Cercek noted that some of the patients with other types of cancer who did not achieve a complete response did experience considerable tumor shrinkage, suggesting they might have benefited from longer treatment. “We also saw lower rates of cancer recurrence, suggesting that even if the effect wasn’t a home run, it helped most patients,” she said
Jemperli was generally safe and well tolerated. A majority of patients had mild to moderate reversible adverse events (60%) or no adverse events (35%).
“This study shows that immunotherapy can replace surgery, radiation and chemotherapy for mismatch repair-deficient solid tumors, which could help patients preserve their organs and avoid the harsh side effects of chemo and radiation,” Cercek said. “Preserving a patient’s quality of life while also successfully achieving positive results in eliminating their cancer is the best possible outcome. They can return to their daily routines and maintain their independence.”
Click here to learn more about cancer immunotherapy.
Click here for more news from AACR 2025.
- #AACR 2025
- #cancer treatment
- #checkpoint inhibitor
- #colon cancer
- #immunotherapy
- #Jemperli
- #rectal cancer